PMDD, Post-natal Depression & Your Anatomy
Premenstrual Dysphoric Disorder
Premenstrual Dysphoric Disorder (PMDD) is a more severe form of premenstrual syndrome (PMS) that affects around 3-8% of women compared to up to 75% for PMS. Women with PMDD experience significant mood swings and irritability that can emerge 1-2 weeks prior to a period and are severe enough to interfere with daily life with symptoms resolving at the start of a period.
Symptoms include:
- Low mood, sadness, hopelessness
- Irritability and anger
- Difficulty concentrating and changes to memory
- Fatigue
- Changes to appetite and sleep
- Decreased interest in usual activities
Why?
The underlying cause for PMDD is uncertain but is thought to be due to sensitivity to normal cyclical hormone changes.
Treatment?
No one size fits all but treatment can include medications that suppress ovulation, selective serotonin reuptake inhibitors (SSRIs), lifestyle modifications, vitamin supplements, herbal remedies and psychological therapies.
Do I have it?
If you think you might be experiencing this it might be helpful to chart your symptoms on a calendar and compare it to your menstrual cycle. It is important to see your health care provider such as your GP to rule out other medical or psychiatric illnesses that can mimic symptoms of PMDD.
Post-natal Depression and Anxiety
Post-natal Depression and Anxiety affect more than 1 in 7 mothers and 1 in 10 fathers and comes on in the first 12 months after welcoming a baby. The anxiety and depression can occur separately or at the same time. Everyone’s experience is different, and symptoms can range from mild to severe is severity. The symptoms can include:
- Low mood or mood swings
- Feeling nervous, having persistent worries, heart palpitations or panic attacks
- Obsessive or compulsive thoughts and behaviours
- Feeling tired
- Issues with sleep
- Changes to appetite
- Loss of interest in things that normally spark joy
- Withdrawing from the baby, friends, or family
- Trouble concentrating or with memory
- Feeling overwhelmed
- Thoughts of harm to yourself or the baby
It is important to know that post-natal depression and anxiety is common and that there are many kinds of support available if you are experiencing these symptoms. Talking to your GP or Maternal Child Health Nurse about how you are feeling is a good start. Other resources include:
- Maternal and Child health line (24hrs) 13 22 29
- PANDA 1300 726 306
- Lifeline 13 11 14
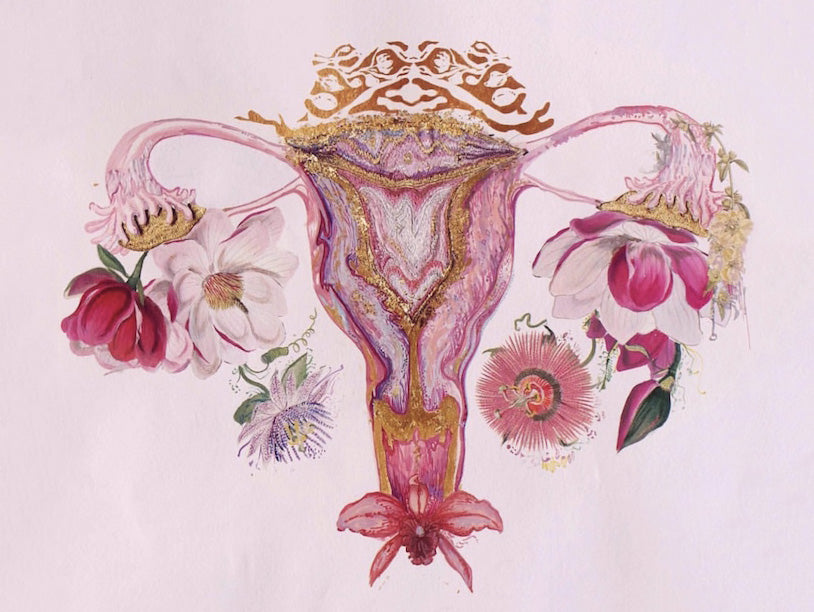
Getting to Know your Anatomy!
The VULVA is a collective term for the outside part of female genitals which includes the labia, clitoris, vaginal opening, and urethral opening.
The labia majora is the two (hairy) external skin folds. They come in many shapes and sizes. Their role is to protect the other external genital tissues and provide lubricating secretions through sweat and sebaceous glands.
The labia minora is the two (hairless) folds of skin inside the labia minora and play a role in protecting the genital structures.
The clitoris is found under the clitoral hood which is formed by the top of the labia minora and plays a role in sexual pleasure.
The urethral opening is a small hole where you pass urine from.
Vulval / Vaginal Health
The vulval skin is a highly sensitive region of our body. There are simple measures that we can take to help keep the skin healthy.
It is recommended to wash the area with either water only, a pH adjusted soap free wash or non-fragranced simple moisturiser once daily.
The following is a list of things that can irritate the vulva skin:
- Soaps, bubble baths, shower gels
- Cleansing wipes and douches
- Regular use of panty liners / pads
- Perfumed products such as washing detergents and softeners
- Feminine hygiene products
- Lubricants and condoms
Try to:
- Avoid wearing tight jeans, pants, or stockings for extended periods of time
- Change underwear frequently, especially if damp
- Choose cotton underwear
- Change out of wet bathers or sports gear as soon as possible
- Wash off water-based lubricants after intercourse
If you are experiencing symptoms of the vulva, please see your GP to discuss further.
Common Conditions of the Vulva and Vagina
Vaginal discharge is normal but if “what is normal” for you changes, it might indicate something else is happening down there. This could be increased amount of discharge or changes to colour, smell, or consistency.
Sometimes sexually transmitted infections (STIs) can cause a change to vaginal discharge, and it is important to see your GP as generally these are easy to test for and simple to treat, but if left untreated can cause long term issues.
Bacterial Vaginosis (BV)
BV is common and is usually experienced as a change to vaginal discharge commonly with increased amount of discharge with an unpleasant fishy smell. It is caused by changes in the normal bacteria that make up the vaginal microbiome. A vaginal swab by your GP will diagnose if you have the bacteria that causes these symptoms. Treatment options including oral antibiotics and vaginal antibiotic creams. Some women benefit form alternative treatments if they experience frequent recurrences. It not considered a STI and partners do not need treating.
Vaginal Thrush
Thrush is a common infection of the vagina and vulval tissues. It is caused by an overgrowth of yeasts that are typically found in the genital area. Overgrowth of the yeast can occur with certain medications, pregnancy and underlying medical conditions. There symptoms include increased vaginal discharge which can be thicker in consistency and the vulva can be red, itchy, or sore. Some women experience pain with intercourse. Treatment includes vaginal antifungal creams or pessaries which are available over the counter at the pharmacy. If symptoms persist, see your GP so they can rule out other causes and prescribe individualised treatment. It is not considered a STI.
Vulval dermatitis
Itchy, dry, or painful vulval skin may be caused by dermatitis. It can things that irritate the skin such as soaps, powders, creams, clothing, douching, feminine hygiene products or lubricants as well as having prior eczema elsewhere on your body. Treatments include avoiding irritants, moisturising and in some cases topical steroid creams.
Book your appointment with our Female GP’s on 03 9132 9644 or email us hello@number1womenshealth.com

